Call to Action
Update AGAIN: The new place to provide public comment by January 16, 2021 is here: https://www.federalregister.gov/documents/2021/02/12/2021-03069/national-vaccine-injury-compensation-program-revisions-to-the-vaccine-injury-table-notice-of#open-comment
The ACCV voted not to remove SIRVA from the Vaccine Injury Table!! Original post below. There is no need to contact the members of the ACCV any longer, BUT PLEASE SUBMIT YOUR PUBLIC COMMENT before January 21, 2021 by following the link above. There is an update about the ACCV meeting here.
There is a proposed change at the U.S. Department of Health and Human Services (HHS) that will hurt the ability of American sufferers of Shoulder Injury Related to Vaccine Administration (SIRVA) to be compensated. The change will take SIRVA off the Vaccine Injury Table. (Watch an NBC News update on this here.)
Since the people who give the shots incorrectly are not liable for the injuries they have caused, due to federal vaccine law, the Vaccine Injury Compensation Program (VICP) is currently the way to get reimbursed for expenses, pain, and suffering.
I have heard from so many of you with devastating financial hardships as a result of SIRVA. For some, it’s being unable to work at your job; for others, it’s bad medical insurance that means high costs for treatments, or traveling far from home to find a doctor who has even heard of SIRVA. For me, I estimate I’ve lost about $20,000 in out of pocket expenses at this point, and I’m still not completely better, 2.5 years later. The VICP is a lifeline here in the U.S. for the (slow) process of getting fair compensation for our costs and suffering.
Please read the information below from Leah Durant, PLLC, and if you can, take the time to make your voice heard! While Leah says this will not affect cases that are already in progress, we owe it to all future recipients of SIRVA to take action immediately to stop this change.
Letter from Leah Durant:
I am writing today to inform you of a crisis within the Vaccine Injury Compensation Program and I need your help, and your voice, today.
On March 6, 2020, at a meeting of the National Advisory Commission on Childhood Vaccines, representatives of the Secretary of Health and Human Services (HHS), unveiled a plan to REMOVE ALL SIRVA CLAIMS from coverage under the Vaccine Program. While attorneys like myself and others have been working extraordinarily hard to get the best results for each and every one of our clients, bureaucrats at the Department of Health and Human Services and lawyers at the Department of Justice have been feverishly working behind closed doors to ram through a regulatory change to do away with SIRVA claims altogether. Their plan is to have this change implemented very quickly and quietly, before too many people know about it.
Because HHS is unable to keep up with the number of SIRVA cases that have been filed, their proposed solution is to eliminate SIRVA altogether, thereby depriving people like you of your right to recover for severe shoulder injuries that result after vaccines.
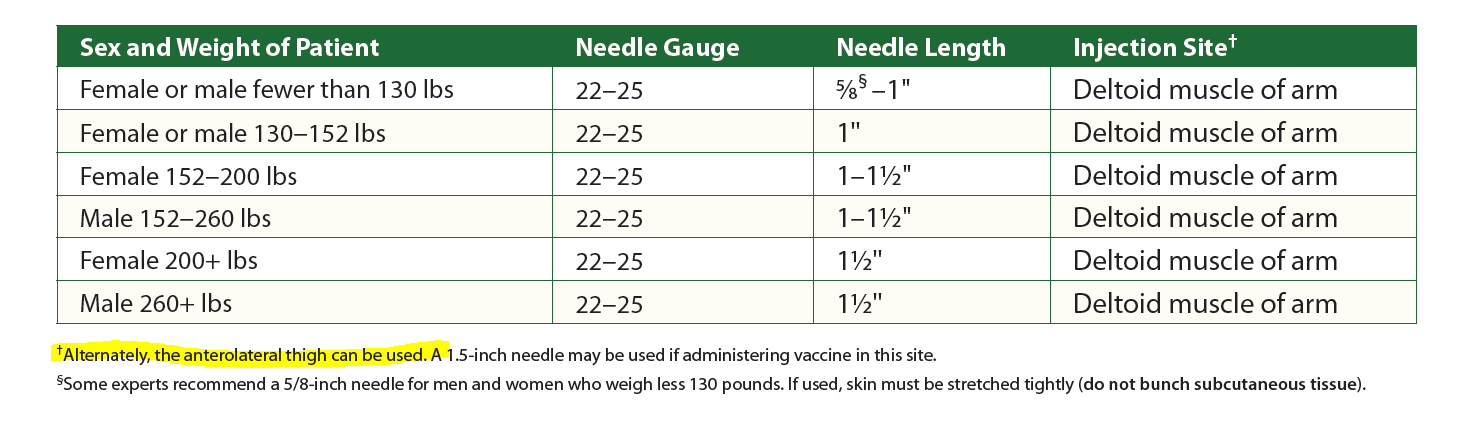
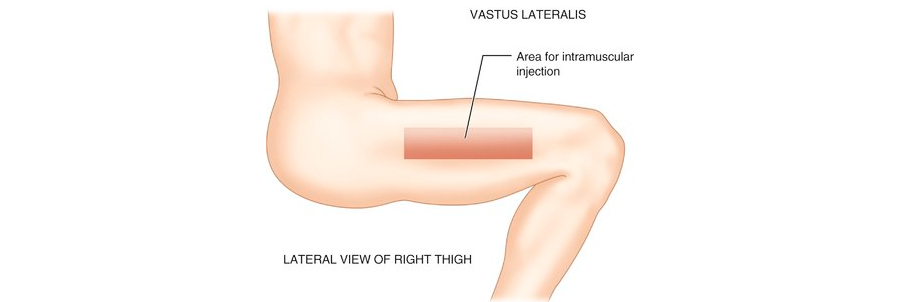
Government officials know that SIRVA occurs frequently and the science behind it is sound. However, rather than working with the CDC to train administrators on how to administer shots correctly, HHS’s “solution” is to remove SIRVA from the Vaccine Program altogether, taking away your right to receive compensation under the Program.
HHS’s plan of action is appalling. The worst part is that they are doing everything within their power to make sure no one is aware of the change, and have unleashed this proposal at a time when the entire world is grappling with a public health crisis. Low-level bureaucrats at HHS want to make their lives easier by eliminating your right to gain compensation for shoulder pain that occurred as a result of someone else’s mistake.
Also telling is that HHS has revealed this plan late on a Friday afternoon, just when the coronavirus crisis is of critical concern and all the high-level officials at HHS have directed their attention to this national emergency. The Commission chairman would not even allow any discussion at the meeting on HHS’s plan. HHS is required by law to allow for a public comment period of 180-days; however, in an effort to make this change at “warp speed,” HHS is refusing to provide any additional information so that the public can know what is going on.
Below are the action items you can do now:
There are things you can do right now, and all week long – until our next meeting, to help the effort to stop HHS from adopting the proposed Rule.
- On the HHS organization chart, the Vaccine Injury Compensation Program falls under the umbrella of a particular Division, the Health Resources and Services Administration (HRSA). It is vitally important that HRSA’s Administrator, and his two Deputy Administrators, are barraged with letters, emails, and phone callsopposing the change. The Administrator at HRSA, Mr. Thomas Engels, is the newly appointed HRSA Administrator (appointed in late November 2019), and I believe Dr. Engels has no idea what is happening in his Division to secretly push this plan through. Your assignment for this week (further assignments coming each week) is to please write letters and send emails to Mr. Engels (from Wisconsin) and his deputies, Brian LeClair (from Minnesota) and Diana Espinosa and let them know how you feel.
Harness the energy that you expressed in Friday’s call and let them know how SIRVA has affected you and why you want all Americans to have the legal recourse you had. Get your friends and family to email and write letters too. We want the snail mail and email boxes of these three people to overflow with our outreach!
And please also do the same for the Secretary himself. All 4 of these HHS officials are vital for us to contact and only Secretary Azar and Administrator Engels probably have the power to turn this thing around at this point.
The phone number for all three of these HRSA Administrators is: 301-443-2216
Dr. Thomas J. Engels
HRSA Administrator
5600 Fishers Lane
Rockville, MD 20857
tengels@hrsa.gov
Mr. Brian LeClair
HRSA Deputy Administrator
5600 Fishers Lane
Rockville, MD 20857
bleclair@hrsa.gov
Ms. Diana Espinosa
HRSA Deputy Administrator
5600 Fishers Lane
Rockville, MD 20857
despinosa@hrsa.gov
The contact information for Secretary Azar, the very top person at HHS, is as follows:
Alex M. Azar II
Secretary of Health and Human Services
Office of the Secretary
330 C Street, SW
Washington, D.C. 20416
Secretary@HHS.gov
Phone Number: 202-690-7000
- Please also write the Chair of the Vaccine Commission with your opposition:
Cody H. Meissner, M.D.
750 Washington St # 213
Boston, MA 02111
- If you are interested in FB and in organizing by state, please contact me [Leah Durant] directly. In this regard, as mentioned above, any of you from Wisconsin or Minnesota that know Brian LeClair (former Minnesota State Senator) or Dr. Thomas Engels (former Assistant Deputy Secretary at the Wisconsin Department of Safety and Professional Services and Vice President of Public Affairs at the Pharmacy Society of Wisconsin) please let me know.
4. Written below are several talking points for your emails and letters to Secretary Azar, Mr. Engels, Mr. LeClair, Ms. Espinosa, and Dr. Meissner.
Feel free to say whatever you’d like, however, please note that all emails and calls will be most effective if they come directly from you. Thus, in order to have their greatest impact, calls and emails should avoid mention of me [Leah Durant], or my firm.
Just let them know that you do not want SIRVA removed because it is a serious and debilitating injury. Tell them what SIRVA has done to you and that you do not want others to be deprived of a path to recover. Tell them that this injury may well affect you and those you love for many decades to come. Please don’t get into the specific details of your case – just that you suffer from SIRVA, that it has altered your life negatively, and that you strongly disapprove of HRSA’s efforts to remove SIRVA from the Vaccine Injury Table because it runs contrary to our nation’s health policy to encourage people to get vaccinations.
HHS’s proposed Rule is not in the interest of the nation’s health policy – we should be encouraging people to get vaccinated, not raising doubts about the safety and efficacy of vaccines. In addition, tell them that you plan to begin contacting your Members of Congress, and you resent that this change is being made in secret and behind closed doors.
######
Thank you all so much for all you are doing. Although HHS is trying to do this without discussion, let’s bring some SUNSHINE to the issue. #SunshineonHHS!
With my best personal regards for your continued safety and health,
Leah V. Durant
Principal and Owner
Law Offices of Leah V. Durant, PLLC
Ldurant@Durantllc.com
Additional Information:
Science magazine article about this proposed change
Open letter from Johns Hopkins shoulder surgeon Dr. Srikumaran [pdf link]
Text of proposed rule [pdf link]
Yahoo Finance article
NBC News video on the change







 Hi all. Welcome to the Summer 2020 roundup of the latest news, articles, and information about Shoulder Injury Related to Vaccine Administration (
Hi all. Welcome to the Summer 2020 roundup of the latest news, articles, and information about Shoulder Injury Related to Vaccine Administration (