
If you’ve landed on this website, maybe it’s because you went in for a vaccination, you were surprised to find yourself still in pain more than 3 days later, and you searched for information about why your shoulder still hurts. I did a lot of that in the days and weeks after my flu shot, when it became obvious that the usual soreness should have passed already. Then I learned about SIRVA.
There are a few articles about Shoulder Injury Related to Vaccine Administration (SIRVA) in newspapers and in peer-reviewed scientific journals. I have provided links to those on the Resources page, and will continue to update that page whenever new articles come out. This post is my summary of that information, after reading and poring over everything I could find. If there’s something medically incorrect here, please, correct me in the comments! I am not medically trained, although I am a scientist and can distinguish between reliable and unreliable sources of information.
Anyway, welcome to this website, and please leave a comment to say “hi” and tell me what you know about SIRVA. If you have SIRVA, please consider taking the SIRVA Survey! It’s private and anonymous. Only by gathering more information can we begin to understand this condition better, together.
What’s going on in my shoulder?
SIRVA is thought to be an immune response to the active agents in the vaccine, which results in inflammation, excess fluid where it doesn’t belong (bursitis), and potentially (in the worst cases) even more damaging effects to the tendons and bone. These features are often visible on MRI and ultrasound imaging, although bursitis and other tendon issues may have pre-existed before your vaccine but were previously not causing you any pain.
With the added inflammation and fluid often comes impingement, which is when certain things get pinched in the tight shoulder joint. Before your SIRVA started, you probably had just the right amount of space for all the bones, tendons, nerves, etc. in your shoulder joint. Now, the fluid and inflammation take up extra space and stuff starts rubbing wrong. It results in the sharp pain you’re feeling on certain movements. Frozen shoulder is also sometimes an associated side effect of SIRVA.
What causes SIRVA?
By this point in time, it SHOULD be well known in the medical community that injecting a vaccine too high on the shoulder will put it into the bursa space (subdeltoid or subacromial) or other part of the shoulder where it doesn’t belong. However, many people who are trained to give the shot are unaware of the dangers (50% in one study). SIRVA can be caused by any vaccine, but it is thought that having previously received at least one dose of the same vaccine increases the risk.
The difference between a properly administered shot (in the deltoid muscle) and improperly administered is that the muscle is highly “vascular” (good blood flow) and the vaccine is designed for that system. In your bursa, in your shoulder joint, it is far less vascular and the body isn’t prepared to deal with the highly “immunogenic” agents in the vaccine. So it fights it, but unlike your body fighting it safely in the muscle, it leads to the undesired symptoms and potential damage described above.
What can I do about it?
Because there are several ways SIRVA manifests in the body, there are multiple possible ways to approach treatment. I can’t tell you what will be effective in (a) reducing your pain or (b) hastening recovery to full shoulder health. I will tell you what I’ve tried, and if you fill out the SIRVA Survey, I will let you know what has worked for other people in future blog posts!
Anti-inflammatories: You might want to start these, if you haven’t already (UPDATE: I’m not sure THAT was good advice, I took them for months before hearing the opinion that they can potentially block the appropriate signals your body sends to injured areas. My primary care doctor and first orthopedist recommended them, but my current doctor doesn’t. Consult your doctor.) Because of the strong inflammation component of SIRVA, they are likely to help cut the pain (UPDATE: but maybe not promote healing). I chose Aleve (naproxen) over Advil (ibuprofen), because I’ve previously found it works better for me (I don’t know why).
Ice: A lot of people recommended icing for 20 minutes 3 times a day. As SIRVA drags on for a while, that becomes pretty difficult to do every day (for me anyway), but I try to apply ice after doing anything that aggravates the shoulder or causes pain. I don’t notice that it makes any difference.
Physical therapy: Frozen shoulder is a common outcome of SIRVA, so getting on top of PT soon is a good idea. It can also help a lot with some associated imbalances and tension that may occur from using your painful shoulder. I don’t know if it’s helpful by itself, given the biochemical nature of SIRVA, but it’s worth a try. Unfortunately, there is probably not one standard way a PT will approach SIRVA cases, with so little information out there. There are standard approaches for subacromial bursitis and for frozen shoulder.
Cortisone shot: You might be reluctant to get another shot when your whole problem was caused by a shot in the first place. I was. But some people find relief, or even complete recovery from SIRVA symptoms (!), from cortisone injections. I had high hopes for this and was disappointed to find absolutely no improvement in my case, and there are possible negative side effects of cortisone shots themselves. In consultation with your doctor, you should consider it, but be prepared (emotionally) for either outcome. I have heard it said that you should see an orthopedist for your cortisone shot and not your primary care doctor (to ensure accurate placement). Some doctors will even do ultrasound-guided cortisone injection, but mine didn’t.
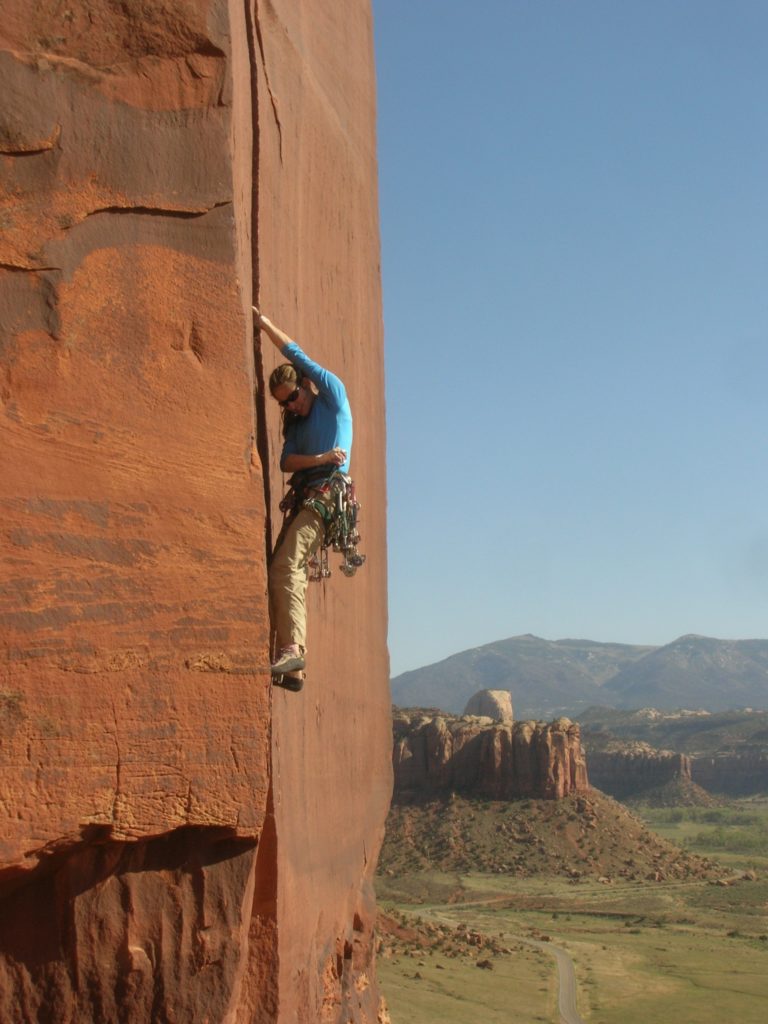
Rest: Unfortunately, this is the one everyone recommends: I have heard from multiple medical practitioners that you should avoid doing the motions that hurt or aggravate your symptoms. For me, that’s rock climbing, my absolute favorite thing on the planet to do, but for you it might be swimming, tennis, reaching for things, whatever. I wish I could do a controlled experiment where I kept rock climbing in one case and rested in another, and see if it makes a difference (since it is a chemical response), but I didn’t want to risk it.
Surgery: I ended up having surgery. I have a couple of posts discussing this difficult decision, here and here.
Running: One doctor theorized that running might help, since it involves pumping the arms (encourages fluid movement in the joint) without overhead motions. If it hurts, don’t do it, but if it doesn’t hurt, maybe it’s worth a try. I’m going to give a go, even though I don’t enjoy running very much.
What does the CDC have to say about SIRVA?
The Code of Federal Regulations (CFR), Title 42, Part 100, discusses recognized injuries from vaccines and the compensation that sufferers are eligible for. SIRVA is defined there as:
(10) Shoulder injury related to vaccine administration (SIRVA). SIRVA manifests as shoulder pain and limited range of motion occurring after the administration of a vaccine intended for intramuscular administration in the upper arm. These symptoms are thought to occur as a result of unintended injection of vaccine antigen or trauma from the needle into and around the underlying bursa of the shoulder resulting in an inflammatory reaction. SIRVA is caused by an injury to the musculoskeletal structures of the shoulder (e.g. tendons, ligaments, bursae, etc.). SIRVA is not a neurological injury and abnormalities on neurological examination or nerve conduction studies (NCS) and/or electromyographic (EMG) studies would not support SIRVA as a diagnosis (even if the condition causing the neurological abnormality is not known). A vaccine recipient shall be considered to have suffered SIRVA if such recipient manifests all of the following:
(i) No history of pain, inflammation or dysfunction of the affected shoulder prior to intramuscular vaccine administration that would explain the alleged signs, symptoms, examination findings, and/or diagnostic studies occurring after vaccine injection;
(ii) Pain occurs within the specified time-frame;
(iii) Pain and reduced range of motion are limited to the shoulder in which the intramuscular vaccine was administered; and
(iv) No other condition or abnormality is present that would explain the patient’s symptoms (e.g. NCS/EMG or clinical evidence of radiculopathy, brachial neuritis, mononeuropathies, or any other neuropathy).
The CDC is well aware of SIRVA (e.g., presentation pdf), but avoids mentioning it on its pages about possible vaccine complications (e.g., here). A lack of knowledge about the problem, even among health care providers, contributes to its ongoing recurrence. Please write the CDC, everyone, and encourage them to take further steps in promoting good practices for administration of vaccines. If you have ideas about how else to get the word out, please let me know!
thanks for creating this page. I am only 12 days in and it has been hell. It was a relief to get a confirmation that it was the vaccine, but now I wonder what the road to recovery entails. I will follow up with your surveys.
Thanks Nicole. If I were you I’d keep hope up that your case will resolve quickly. Some folks get better in under 3 months. Please keep me posted!
I have suffering from SIRVA since Nov 2019. Still not 100 % back to normal
Me too. November 2019 and after getting a little better but plateauing, decided to try Tenex to speed recovery. That was Jan 2021. Now I’m pretty much as bad as I’ve ever been except for maybe the first few weeks. ☹️
What a nightmare! M&M size complete rotator cuff tear, bursa fluid, muscle & tendon impingement and early degenerative bone disease of the AC joint. If the doctor would have said “agree to a couple vaccines and you might end up without a limb” my reply “no way”! Depressing when you ask doctors and nurses if they are familiar with SIRVA and every one of their replies “What’s SIRVA I do not have a clue”. When one is up sleepless nights one has a lot of time to surf the web and learn a lot. Got the bad jabs in 2017 – will never get another – no amount of money justifies the loss of your limb and the misery of a bad jab for life from a vaccine; my opinion for myself – yes I have filed a SIRVA claim – and everyone be smart when you get vaccinated and be safe my friends!
where do you file a SIRVA claim –
Debbie, if you google for SIRVA you will find a lot of webpages of lawyers who specialize in the vaccine injury courts. For example,
https://vaccinelaw.com/
I would recommend trying to get in touch with a few of them to figure out who is responsive and who you like, then, if they agree to take your case, they will have you sign paperwork and they will file your claim for you. You need to have been injured for 6 months before a claim can be filed.
If a claim is successful, what does it cover? Is it just medical expenses or does it also compensate the individual for pain and suffering?
I’m a little over 2 months in and I can’t imagine living like this forever.
Hi. I live in Canada and there doesn’t seem to be much knowledge about SIRVA. My flu shot was 6 months ago and I am in agony. At the time I knew it was administered too high.
Have been to PT sessions, taken celebrex, and rested. I prefer heat therapy. I am feeling helpless right now and the inflammation is affecting my health. Thank you for your info.
How did you get a doctor to confirm that it was a vaccination shot that caused your injury? It’s almost 4 months later and my doctor is not helping me with this.
Hi David. Agreed. Getting help from the doctors I’ve worked with has been difficult. They want to treat the SIRVA like a frozen shoulder although they agree it’s not. I looked into doing a video visit with one of the doctors on the map (Eric-something at NYU)…
I’m journaling about it as much as I can. Also, I filed a “complaint” with my health system. At first, I got a letter back that was totally dismissive. Now that I’m four months in and started working with a lawyer, I am getting a little more interest. Amy…thanks for this site. It’s been a godsend. I have a whole new understanding for what pain can be.
Hi Colleen. Thanks for reply. I have tried several approaches to find help regarding my shoulder. My doctor treats me like I did something to myself. I’m at the point of looking into disability as it’s about to take my career. I need a doctor who will believe me and shows some concern
I hope you found help, David. Maybe the doctor you tried is in cahoots with whoever did your vaccine?
This whole thing is awful, how can so many professionals be untrained about this ?
I received the flu jab six weeks ago, and am still in considerable pain. Pain killers have no affect at all, I am getting little sleep, my GP has offered nothing that can immediately help, but will refer me to a physiotherapist.
Jackie, sorry to hear that. I hope you find a good physiotherapist who comes up with a helpful treatment plan. An orthopedist referral would also be good for you to get from your GP, and an MRI. In my experience, without knowing exactly what inside your shoulder the shot hit (maybe possible but hard to tell based on your physical symptoms alone by a good PT), the PT may not be able to design an ideal program for you. They will have better resources at their disposal if you have even more information. GOOD LUCK!
yes, I found that OTC pain pills did not work. Ice helped A LOT. I am still dealing with this 5 months later. Don’t have a cure yet. Can’t put on my jacket or take it off without pain among other things. Can’t lay on my left side without trying to find a position that does not hurt.
I know. Same thing for me now going on 6 months☹️. I find the mornings are the worst from unintentionally sleeping on my arm. So frustrating this has happened.
I am in Ontario. Developed the pain a couple of weeks after the vaccine. So incredibly painful. It’s been 6 weeks and moderately better. Toradol is the only Med that works for me
Elaine, I have had the same, and I’m in Alberta. It’s been 6 months, there is no program in Canada that I can find for compensation for vaccine injuries, and little knowledge about it. Worried about getting a covid vaccine while this arm is still affected, and I can only do the one side.
I have the same Symptoms for nearly 6 months now my left upper arm my muscles are so weak and injected site it’s so painful touching the area , that normally will be fine , I have stabbing / throbbing pain all the time in my left arm , Decreased range of motion and I have lose mobility in my injured arm. … pain is severe all the time it’s unbearable , what bad luck of getting SIRVA injury, I knew right from the start she did my vaccine wrong as it hurt so much putting the vaccine in my left arm.
I had a flu shot in the middle of Oct. 2018 and am still experiencing pain in my left shoulder down to my elbow, my neck and a lump/knot popped up on my shoulder blade. Ice/heat/Aleve help for a little while but pain never goes away, even just sitting still at rest. I had NO pain prior to the flu shot. I am 63, on social security with no insurance. Had the flu shot at a local Walgreens Pharmacy. I do not know what to do now.
Kathy, I know what you mean about the “knot” or lump in your shoulder blade. That’s been a constant companion for me too. I don’t think it’s directly related to the injury from the shot but is from tension/compensation of the other rotator cuff muscles as they try to protect the injured ones closer to the joint and injection itself. I am feeling it right now as I type this, too. I also find that it can be temporarily alleviated with Aleve and ice and heat and massage. I think maybe PT can address it as well. It is very, very annoying and often (for me) more persistently painful than the primary injury area (which hurts more with certain motions). UGH!!
As far as your next steps I am afraid I don’t know much about health insurance while on social security and past a certain age but if you can’t afford to see an orthopedist and get an MRI and get good targeted physical therapy (which would be my recommendation), I would at least try to get one appointment with a really good PT to get some idea of stretches you can try.
You should talk to a vaccine lawyer (lots of them come up when you google SIRVA) but I think they will tell you two things: 1. you have to be injured for 6 months before they’ll talk to you seriously about becoming a client, and 2. you should get the care you need (which takes $$$) and hope for reimbursement later, likely much later (1+ years IF your case goes well). #2 isn’t helpful if you don’t have the money right now of course. I am sorry.
Finally (and this is poor consolation) you should know that those of us who are doing all those things that require good health insurance aren’t necessarily getting better any faster…I’m over a year out and still injured and that’s with a LOT of care (orthopedists, PTs, etc). No one really knows how to treat it best anyway, which is what I’m hoping this website and survey will help with eventually. That is a depressing way to wrap up this comment but sadly it is true: some SIRVA cases get better in fewer than 3 months without intervention (I hope that is you!!), some cases turn into frozen shoulder (PT can help avoid that), some cases have resulted in damaged structures that would improve better with surgery (e.g. rotator cuff or bursa), some people get relief from cortisone injections but not all, etc.
My pain started 5 days post vaccination in the opposite arm than the injection. It quickly spread to both with what felt like my muscle’s were being shredded from elbow to upper arm. Horrible pain could barely move arms. This lasted about 65 days, pain then changed to a pressure (like a BP cuff left inflated on arms. It is 5 1/5 months of dealing with
This. Wondering if I should have gone to an orthopedic doctor at the start instead of my GP who was of no help.
Maybe I could have been treated with prednisone or cortisone to slow down what was happening to me.
Thank god , I have found others that have had these side effects, even with the pain starting in opposite arm from the one that was injected. This at least has helped my mental status some.
It’s been about 1 yr for me but have not been diagnosed with sirva. Was told it’s shoulder impingement. Had steroid shot and saw a chiropractor. I had never heard of Sirva until our local tv station did a story on it. Have another appt w orthopedic doc Jan 14th.
Good luck Brenda—after a full year that sounds pretty likely that it is SIRVA. Sorry it has been so long for you in getting the right information; it is awful that so many doctors are unaware. When you see the orthopedist on the 14th you might have to be ready to convince him or her, too. It’s exhausting. I hope you find this helpful:
http://sirvasurvey.org/talking-to-doctors-about-sirva/
Hi. I had the flu jab 2 weeks ago. Have never had a reaction to it before. I’m 69 years of age but very fit. The next day I was in agony with my shoulder and could not take a tee shirt off without my wife’s help or wash my face as I had to lift and bend my arm. After a few days it eased considerably. The pain in the shoulder stayed though and never went fully. It’s now been 3 weeks and if I do certain actions it hurts a lot. An example is flicking the duvet cover off myself using my left shoulder. Raised positions hurt and sometimes hurt a LOT. I can, however, at the minute anyhow, hit a golf ball and ride a bike. It doesn’t actually hurt when I do these but not sure if it may aggravate it. Will check with my doctor now (it was the pharmacist who administered the jab though) and explain what has happened. I will pay privately for a scan to see what’s going on as my whole life revolves around being physically active. I need to get it evaluated as there is just no improvement. I am used to injuries and what my body feels like and because of the timing of this I’m convinced it’s something to do with the flu jab.
Hi Roger, sorry about your case – some of the symptoms sound really familiar – like the duvet cover. Adjusting the blankets at night was very painful for me right away.
I’m glad you’re still able to do some of your activities and I don’t have a good answer for the aggravate question. I kept active (running and biking) as much as I could, as well. (Had to stop rock climbing, though.) For nothing else, it makes the experience a little less miserable, if it takes a while to heal.
Since you’re still early, there’s hope that your pain will resolve quickly. Some cases do resolve within a few months. Good luck and please keep us posted!
I had the Covid injection approximately 10 weeks ago.
I started to experience sharp pain and restricted movement the following day.
I can’t even put a grip in my hair!
What’s made it worse, I am right handed, a the injection was put in right arm.
I am waiting for the telephone
appointment with Dr.
Interesting. I just had mine on 10/21 and it was still bothering me (same symptoms as yours) a week and a half later so I messaged my doctor this week and was told ice and ibuprofen/aleve and let them know if it didn’t get better after a few days. Went to the doctor today (unfortunately, my normal primary isn’t in till mid month) so had to see someone else. I had found information about Sirva and when I mentioned it, they didn’t know what I was talking about. Wish my doctor would have been there, feel like she would have listened a little better. Anyway, gave me some exercises to try and said to contact in 4-6 weeks if I’m still having problems. I guess time will tell. I feel like it’s aggravated more after the appointment. Was told deltoid/rotator cuff.
I had mine in Oct 2020…still having pain in March 2021! working with Doctors so far trying ice, sling wearing, anti-inflammatories, muscle relaxers, and soon prednisone (one at a time more or less).
Hi Amy
Thanks for this resource – it’s really informative and makes the best of a terrible situation.
I’m 3 weeks in. Had 10 days of Arcoxia 90 mg. Worked like a miracle, then the original pain and discomfort came back swiftly after the last dose of Arcoxia.
My diagnosis was bursitis with a frayed tendon based on MRI.
The good news is that the MRI does not show a torn or ruptured tendon, but I don’t know whether the tendon damage will increase with time due to the inflammatory reaction (do you know?).
Was quite concerned to read about the possibility of bone damage / edema.
How often does this occur? I guess I don’t have this yet as the radiologist did not mention it in the report. What can I do to reduce the likelihood of it happening?
Any other advice would be so much appreciated.
My response to this comment actually showed up under your very last comment, so check there for my advice 🙂
Cheers,
Amy
Hi again Amy
In addition to seeing an orthopedic doctor, have you or anyone you know of seen a rheumatologist?
I actually think SIRVA straddles two medical specialties. Whilst the damage is physical, the cause is biochemical.
The orthopedic doctor is great for the first, whilst rheumatologist would be much better for the second.
An immune response which results in the body attacking itself is essentially what the rheumatologist does (and is what SIRVA is).
The risk is that the orthopedic doctor focuses on physical healing, but is not accustomed to thinking about ways to stop the underlying cause (which is not physical). A wonderful knowledge of shoulder anatomy doesn’t really help to do for reasons mentioned.
I didn’t see a rheumatologist but I think it is a great idea, especially if you live in an area where you can find a rheumatologist who is excellent and interested in problems that are maybe a bit on the edge of what they normally study (but as you say, potentially related by the sort of biochemical/physiological behavior). I wondered out loud to a couple of doctors whether the better way to think of it is “we need to dampen the immune response” to make the injury heal (i.e., get the body to stop attacking the antigens), or “we need to strengthen the immune response” to make it heal. I don’t know that I ever got an answer but a good rheumatologist might know more than the average doctor or orthopedist about that question. Please do try it out if you have the opportunity, and let me know what you learn!!!
Hi Amy, I fully intend to see a rheumatologist.
In my country, there are several. They are all fully booked and I was not able to get a slot today. But I have an appointment scheduled for next week.
Part of the reason I thought about seeing a rheumatologist is because the orthopedic doctor (who has a shoulder sub-specialty) kept going on about wear and tear and was very afraid to commit to a view that it was SIRVA — even though we all knew it probably was this.
He was certainly medically competent in my view. But I guess where financial incentives lie, his business depends much more on GP referrals than me. So I think that would create a disincentive to say or write something which I could use as a basis for a medical negligence claim against the GP. In fact he absolutely refued to put anything in writing. (GP stands for general practitioner, the equivalent of an “MD” in the USA).
The radiologist on the other hand had no such financial incentives, and his written MRI report actually said that some of the injuries could have been caused by an inflammatory reaction due to vaccine.
Hi Amy, assuming the MRI scan done 11 days after the vaccination only showed tendon fraying and no other damage, do you know if the inflammatory reaction will cause further, more serious, damage (e.g. rotator cuff and tendon tears) with time?
Or is it generally the case that the damage is constant?
Hi David, thanks for the comments. I’m not sure about the likelihood of the tendon damage worsening, but I’d definitely suggest advocating for getting an MRI again in a few months to monitor the situation (including both keeping an eye on the tendon and the possibility of bone marrow edema growing between now and then). I think bone edema is very common in SIRVA cases. Before starting the survey I crunched the numbers from the medical papers and it was about 30% of the reported cases that mentioned bone changes—but it may be a biased sample of course because perhaps only the “worse” cases make it into the literature.
I don’t think the physiological mechanism that causes the bone damage from SIRVA is well understood. In the Salmon et al 2015 paper (linked on the Resources page) he lists 3 possible hypotheses for what causes the bone damage. He seems to lean towards this one: “The third hypothesis is a direct mechanism by injection of the vaccine to bone contact [10]. The local inflammatory reaction is responsible for erosion and edema of the upper outer of the humeral head.” I don’t think that provides any guidance for prevention of the slow growth of an edema in the humerus if it is going to happen, except maybe you should talk with your doctor about really stifling the inflammation. I thought I was going that route (sort of) with both steroid injections and ~2 months of large doses of NSAIDs but it certainly didn’t prevent it in my case.
Based on what I’ve learned so far I’d guess that if you are still symptomatic in a couple of months the best course of action MAY be to have an excellent orthopedist go in and “scope” it out. Once in there they can do what they would typically do based on the severity of damage they observe, whether it’s a bursectomy or rotator cuff repair. Recovery from a bursectomy and debridement only of the rotator cuff should be relatively fast as far as surgeries go. But the thing to be hopeful about is that your symptoms will resolve in the 3-4 month timeframe which is also pretty common. GOOD LUCK!!
Thanks Amy. I’m looking forward to the 3 -4 months to see if it will get better.
The pain came back much worse after disappearing when I was on Arcoxia 90 mg. This made me wonder if the treatment was effective for the underlying cause in the first place.
Is the surgery you refer to keyhole surgery?
Yes, it would probably be arthroscopic surgery, at least mine was, nd the way my orthopedist phrased it is “we’ll just see when we get in there what the right course of action is”. He ended up only taking out a bit of the inflamed bursa (as opposed to the whole thing—my shot missed more of the bursa and hit at the teres minor attachment to the humeral head), debriding the frayed teres minor, and taking bone biopsy but otherwise not touching bone other than to observe that it was “soft” and yielded too easily under the awl.
Yeah, interesting observation about the medication. I stayed on NSAIDs for about 2 months (440 mg sodium naproxen 2x/day) and certainly felt no better when I came off them, and my pain also got worse after that long before it got better. Also suggests it was not helping any part of the underlying cause as well.
Hi Amy
I thought further about the rheumatologist. I have a confirmed appointment in a few days’ time.
I know for a fact that people with rheumatoid arthritis (RA) take immune system suppressants. See “Methotrexate” on Wikipedia, for example.
Concetually, RA is similar to SIRVA — the immune system attacking the body.
Of course, the causes and triggers are totally different. But the mechanism of destruction of body parts seems very similar (once triggered).
If the treatment for RA is to suppress the immune system, logic suggests SIRVA should be treated in the same way. Or rather, I cannot think of a logical reason why it would be treated in the opposite way — i.e. boosting the immune repsonse.
What do you think?
I feel the orthopedic doctor did not carefully apply his mind to the immune system as the trigger for this reaction.
I’ll keep you posted.
I thought about this a lot too when I was considering stem cell injections, which are essentially boosting the immune response, by providing the raw materials for immune system activity directly to the site of injury. The way I thought of it is: If there is a battle going on in your shoulder between your immune system and the antigenic agents in the vaccine, and your healthy tissue is the collateral damage, then is it better to avoid collateral damage by (a) making your immune system walk away from the battle altogether (i.e. suppress it) or (b) boosting your immune system to go ahead and win the battle faster and get back to healing?
Here is how I posed that question to a doctor by email: “My biggest question is whether you think there is any risk that a BMAC+PRP [stem cells] injection could increase the body’s immune attack on its own cells, i.e., if there is any chance it could inadvertently make things worse. If SIRVA is the immune system mobilizing to fight the antigenic agents of the vaccine, and its cause is inflammation/collateral damage of healthy cells while the immune system fights the antigenic invaders, then is there any chance (based on what mechanisms are thought to be active in PRP and/or BMAC) that this process could be “helped” by the injection and it might make things worse? Would it make a difference if we knew whether there was any remaining antigen in the originally-affected tissue or if the continued, long-term pain is at this point a residual of the earlier immune system battle?”
The doctor didn’t give an answer directly at that time; he wrote: “These are good questions. I don’t know the answer. I got an email today relating to MSCs (mesenchymal stem cells, the ones we get from bone marrow) being involved in a positive way with regard to infections and the immune response. I’ll dig up the article and send it to you. Arnold Caplan, PhD, of Case Western Reserve University, is the MSC expert and talks about the MSCs protecting structures from an overactive immune system. I’ll email him and see what he says.”
I didn’t hear back from the doctor about his conversations with Dr. Caplan but we spoke in person and my recollection is that he said that he believed stem cells could cause a flare in pain followed by dramatic improvement. But he didn’t know for sure, and while he wanted to do whatever I thought was best to get better, he also was interested (from an experimental standpoint) in trying out the stem cells on SIRVA.
I found this quote: ” In autoimmune diseases persistent antigenic stimulation recruits endogenous MSC to the site of lesion that contribute to the fibrotic evolution. Therefore, administering MSC to a chronic inflammatory disorder may not be desirable.” I sent it to the doctor and he responded: “Your situation is not like autoimmune disease. In autoimmune disease, the antigens are always present and present everywhere, whereas in what you have the antigens were in just one place and we think are in decline if not absent as you suggested. The safest and simplest thing to do would be another “wash-out” if you think that helped you before.”
Even though I agree with you that the logic suggests suppressing the immune system and that rheumatologists are the experts at that, I find what seems like conflicting information in the literature but I’m sure that’s an artifact of my not totally understanding what people are talking about. E.g., “Most surprisingly, use of MSCs for in immune-/inflammation-mediated diseases appears to yield more efficacy than for regenerative medicine” (https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-016-0289-5).
Yes, please keep me posted about what the rheumatologist says and about anything else you learn along the way!!!
Hi Amy, thanks for the detailed information on stem cells.
Regretfully, it sounds pretty speculative and, on balance, I wouldn’t feel confident doing it based on the present information.
I can understand why you opted for surgery instead.
Just curious, won’t the immune reaction come back again after surgery? If not, why not?
Your last question definitely stretches the limits of my understanding about how it all works, but I think there are a couple of ways surgery helps. So if the antigenic agents from the vaccine are already gone/dealt with a couple months out, what you’re left with is the pain from that collateral tissue damage, i.e., the frayed tendon and/or bursitis and/or bone marrow edema. In the case of a bursectomy, removing the inflamed bursa appears to relieve the symptoms. When the bursa “grows back” it is healthy.
There are papers about how long, exactly, the antigens from flu shots are retained in the system. There is one interesting old paper where they found that collagen-rich tissue (as opposed to the muscle where the shot is supposed to go) is especially “retentive” of flu vaccine agents, i.e., they stick around longer than when in the muscle, but this was a lab study on rabbits (Cooke et al. 1972): “The retained intraarticular antigen was eliminated very slowly, with a half-life of over 20 days. These data indicate that the chronic synovial inflammatory response is associated with a chronic local immune response in which prolonged active synthesis of immunoglobulin and specific antibody directed against the locally retained inducing antigen takes place.”
A study was actually done in humans and published in 1990 (Trollmo et al 1990). They talk about systemic response to flu shot injection either intraarticularly or subcutaneously (they don’t compare intramuscularly). They write: “There are at least two possible explanations for the observed inerease of antibody response In serum after intra-articular compared with systemic immunization. A unique feature of the
joint tissue is long-term antigen retention in avascular and hypovascular collagen-rich areas (Cooke et al., 1972; Hollister
& Mannik. 1974). This phenomenon is probably due to the
eleclrostatic interaction between the antigen and the cartilage
(van den Berg et al.. 1986). The retention of high amounts of
antigen may facilitate the uptake and presentation process by
antigen-presenting cells. Also, the Arthus-like reaction observed in all the subjects shortly after the intra-articular immunization might have contributed to the enhancement of systemic antibody response by increase of vascular permeability in synovial tissue leading to influx of T-lymphocytes into the joint space. The antigen-presenting cells residing in the synovial tissue would, by the interaction with these T cells, give rise to an efficient immune response in situ.” This would probably be a good paper to show a rheumatologist. (https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1365-2249.1990.tb05458.x)
Thanks for the paper, Amy. I’ll show it to my rheumatologist.
These are the two questions I’ve framed for him to answer.
What can we do to:
(a) calm the immune reaction going on now (not just mask the pain), to prevent further damage to tissue and bone;
(b) reduce the retention period of antigens by tissue in the joint space (i.e. expel the antigens faster)?
I just realised that one of the co-authors of the AFP article (“Don’t Aim Too High”), Dr Sally Ayoub, is a rheumatologist.
So it does seem that seeing a rheumatologist might be appropriate, even though there are no reports of one actually being consulted for SIRVA.
Nice!! Yes, I totally agree that it is a good idea and very appropriate. I hope you end up with a good one and get some good insights and ideas for treatment. Could even be a breakthrough if RA-type strategies have not been tried on SIRVA yet (I haven’t seen any indications of it in the literature). But my only concern is that it sounds like the immune suppressing drugs used to treat serious autoimmune disorders can have major downsides/side effects, which are a fair tradeoff for people with chronic illness but maybe not worth risking for an acute problem. BUT, I know very little about this, and the rheumatologist would all about drugs or treatments that have less risks!! Good luck!!!
Amy
Actually, according to WebMD, a steroid injection IS a form of suppressing the immune system:
“Steroids work by decreasing inflammation and reducing the activity of the immune system. ”
https://www.webmd.com/arthritis/steroid-injections#1
Based on your research, do you think a high proportion of people had success with the steroid injection?
I am quite concerned as my condition has deteriorated so rapidly since I stopped Arcoxia. This morning I could raise my hand 90 degrees, by evening it was just 30 degrees.
I saw Dr. Bodor, who wrote an article in 2007 about his good success rate (in 2 patients) with multiple targeted steroid injections (https://www.ncbi.nlm.nih.gov/pubmed/17064824). When I saw him in 2018 he says he would not recommend the same thing he did back then. I don’t want to put words into his mouth but I wonder if it has something to do with what I said in an earlier comment about tendon damage from steroid injections—my other ortho said that steroid injections to the bursa are considered safer than targeting the tendons, even though once you inject the steroid moves around for sure. I may be misrepresenting all of this.
In the survey, some respondents have tried cortisone injections. Of them, 6 report “extremely helpful”, 9 report “slightly helpful”, 4 report “not at all helpful or harmful”, and 1 reported “harmful/made symptoms worse”. Of course this doesn’t get at the question of whether it’s just pain relief or meaningful improvement. Your finding in webMD suggests a mechanism for it to be actually meaningful.
Thanks for having me look deeper into the Survey responses specific to steroid injections. That gives me an idea to do a full post on specific treatment concepts, like steroid injection, with more survey results. There are also written comments about steroid injections, too many to go into here, but I can summarize them in a post. But they include, “I’ve had two cortisone injections, one on Nov 30 by my primary, one on Feb 14 by the orthopedist. Neither worked, although the one given by the orthopedist helped with pain for a week or so”. Etc.
Thanks so much for digging up your survey results, I appreciate it Amy.
Would it be fair then to say that based on the evidence you have seen, keyhole surgery appears to have a higher success rate the steroid injection?
I also wonder if I did the MRI scan too early (9 days after vaccination) such that the orthopedic doctor’s conclusion was a false negative.
He said it was good news that that only bursitis was present (and he would rate this a 3 or 4 out of 10, relative to all other cases of bursitis), and there was only tendon fraying, but no rupture.
In your case, and many others in the literature, the MRI scan was done later than T+9 days. In that sense, the progression of time allowed more stuff to be destroyed.
I’m concerned that doctors would look at the MRI scan and take a conservative view. But in reality, things have gotten worse inside my shoulder since the MRI scan (the level of pain has certainly increased), which is now almost 2 weeks ago.
Hence the treatment recommended might not be the most appropriate in the circumstances due to inaccurately identifying all injured parts of the shoulder.
Yeah, in my 1 month MRI (technically: 1 month and 4 days) there was also a moderate bursitis signal, nothing extreme, although my orthopedist called it “significant”. We proceeded to treat as if bursitis, including the steroid injection, and PT that focused on bursitis/impingement. Later (4 months in) when I saw Dr. Bodor with the diagnostic ultrasound and he identified the teres minor as the site of the damage, my PT shifted to supporting/helping the teres minor and I believe that shift in PT was helpful—and it would not have happened without identifying the real site accurately. (My PT said to me after we found out, “I suspected that bursitis was not really consistent with your symptoms, but wasn’t going to question the doctor’s diagnosis”). By the time I got the second MRI at 6 months the bursitis signal had basically disappeared, and in surgery at 6.5 months the surgeon found the bursa hardly inflamed.
No one really mentioned the teres minor fraying in either of the MRI reports in my case (which is why when Dr. Bodor found it on ultrasound it was very surprising to me). The surgeon saw it when he was in there.
Anyway, yeah, I agree with your last sentence, but if frequent MRIs are off the table (maybe you can convince your docs for more!), maybe try seeking out someone skilled in diagnostic ultrasound? Apparently not every ortho with an ultrasound is good at interpreting it, so you would want to find someone good. Even though MRI is the gold standard for seeing SIRVA-related damage, the ultrasound was a very helpful key in my case.
Best,
Amy
Thanks Amy. My MRI report said:
“moderate oedema with bursal sided surface fraying involving the left infraspinatus tendon. This is located at the region behind the humeral head. This is centred towards the interior half of the Infraspinatus tendon. There is surrounding overlying oedema. If there is recent injection at this site, this can represent post injection inflammation or reactive change. No loculated fluid collections are seen. Remnant fibres are still seen inserted at the infraspinatus footprint”.
My doctor’s diagnosis was “left shoulder bursitis and rotator cuff tendinosis”.
I am probably going to start seeing another doctor because this doctor was not keen to commit to the reality that this was in fact SIRVA. He spent a lot of time going on about wear and tear, and how bursitis is a result of the frayed tendon (in non-SIRVA cases, tendon damage leads to bursitis, not the other way round).
So I’m concerned of ending up in a situation similar to yours — i.e. bursitis being an inaccurate diagnosis and failing to treat the more serious damage.
Thanks for making me aware of that possibility.
Hi Amy
I saw the rheumatologist. He didn’t say much. But as promised, here’s the report below.
Inflammation will take 6 weeks to settle. There is nothing you can do to speed this up. This 6 week figure is based on injection of some other kind of oil into joints (was not able to understand this part clearly) — not a vaccine.
Whilst on Arcoxia, the pain reduction was due to control of inflammation, not merely the masking of pain. If it were really just the masking of pain, then taking lots of panadol or ibuprofen would have done the job (but it did not).
You cannot let the pain go untreated otherwise the surrounding muscles will become stiff. Your body’s protective mechanism will kick in. This is why you need to take Arcoxia for as long as you experience the pain. Concurrently, do PT.
Taking Arcoxia helps to calm the immune reaction going on in the shoulder (by reducing inflammation). This is not an autoimmune disorder (I think by that, he meant there is no need to take an immune suppressant).
[continued]
It is possible that the inflammation alone caused the frayed tendon (as opposed to wear and tear before the vaccination), but this is hard to know for sure.
In a small proportion of the population, a vaccine can trigger rheumatoid arthritis even if administered to the right location. The fact that it was administered to the wrong location here does not increase that risk.
Whilst on Arcoxia, it should not damage your shoulder if you do movements which would otherwise be painful without Arcoxia, as long as not lifting heavy weights.
Did blood test for some inflammation markers.
Prescribed Arcoxia 90 mg for next 2 weeks, plus Norgesic.
David
Thanks very much for the detailed report, David!
Consulted today with an orthopedic surgeon who’s supposed to be one of the best in my country.
• He has never seen a case of SIRVA and was quick to say this was his honest view. He was sceptical at first. Said any condition can be found if you look hard enough in the medical journals but was quick to clarify that he was “not trying to protect the GP”.
• He said a more major concern would be nerve damage because the vaccination was injected at the wrong place. He confirmed I did not have this. He has seen cases of this before. You will feel weakness and numbness if this is the case.
I think your orthopedist’s comment about “you can find anything if you look hard enough” may well be true, but the number of papers about SIRVA in the literature is surging, not the other way around (e.g., the famous case where a paper claiming a causal link between vaccines and autism had to be retracted for the medical journal: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2831678/). Here in the U.S., I find the paper by Dr. Atanasoff useful to show first because she works for the U.S. Department of Health and wrote this paper collecting 13 cases—i.e., the U.S. government health services doesn’t deny SIRVA’s existence at all, they way they deny a link between vaccines and autism. But I’m sorry the “show the docs some papers” approach had limited success in your case.
The skeptical ortho I saw (#3 in my post about Talking to Doctors about SIRVA) also was at first telling me it was nerve damage. That is a well known complication, I believe, from injecting too LOW, as opposed to too high. Most givers of vaccines, doctors, and orthopedists are aware of this complication—much more aware than of the damage that can be caused by shooting too high.
I have been following this conversation closely. My orthopedist does not believe in SIRVA and so he wanted to inject a corticosteroid without any imaging first. To me, this sounds traumatizing and terrifying. It also sounds like a great recipe for my worker’s comp claim to continue to be denied because now they can claim the steroid injection caused damage if I get an MRI later on with a different provider.
At a standstill, I’ve been looking into other options while I go to PT twice a week. I am going to ask my GP for a referral to a rheumatologist, if for no other reason than to keep proving I’m in treatment to the worker’s comp people and to see if I can get an order for Arcoxia.
Today I sent my ortho a 4th SIRVA article, this one from a radiology journal. I don’t know if he’s just sick of my emails but he finally ordered an MRI. HURRAY! I agreed to get a steroid shot after the results are read. I wish I’d be in better shape for Christmas, but at least things are progressing.
This site makes it a bit less lonely.
Hi there,
I think your reasoning about waiting for the MRI to try a steroid injection is sound. A very recent paper (not even yet added to the resources page) talks about giving two SIRVA patients a steroid injection within 5 days of getting their misplaced shot, with good outcomes, but for most of us we haven’t seen a competent qualified orthopedist within 5 days of our injury, so that’s out of the question:
https://academic.oup.com/milmed/advance-article/doi/10.1093/milmed/usz269/5588762
In terms of the responses from people on this site, steroid injections at a later date seem to be helpful in fewer than half of everyone.
I’m glad you’re finally getting an MRI from your orthopedist. I think David’s idea about seeing a rheumatologist is a very good one too, and I hope you have some luck and it turns out to be helpful—-please report back with what you learn!!
Best,
Amy
Hello,
Thank you for all the work going into this website. I am waiting for my second PT appointment about two months out from a tetanus shot to the right shoulder. The pain has not stopped even after two months. Also, I have reduced range of motion. MRI at five weeks shows partial tear of teres minor tendon.
Mikael, sorry to hear you’ve gotten a SIRVA injury too. Sounds like maybe we got the shot in approximately the same incorrect place, with damage to the teres minor tendon. Please keep me posted on how things progress for you!
I am a 72 year old white male who was in awesome shape. I received a flu shot in my left shoulder bursa on Sept 17,2018 at Walgreen’s and still have pain, dead arm ect. I’ve done Physical Therapy, x-rays with an Orthopedic Surgeon and an MRI.
The problem in Tucson, Az is that the good medical professionals are unfamiliar with SIRVA. Luckily my Doctor and his PA are working with me to find a resolution for the SIRVA damage. I’ll forward this website to them as I have other information concerning SIRVA. I have retained a lawyer to represent me that specializes in SIRVA claims.
He told me the steps my doctors would put me through while searching for a resolution to the damage in my shoulder and was correct.
I would suggest retaining a lawyer to recover out of pocket expenses.
This too shall pass.
THANK YOU for this website! I got my flu shot on September 27, 2018 and still dealing with it. To make a VERY long story short, my MRI (end of Nov) shows bursitis, infraspinatis tendinopathy, narrowing of acromiohumeral interval, edema, etc. But no tear, so that’s good! I’ve done PT, two rounds of oral steroids and one cortisone shot. My ortho doc (who has been WONDERFUL) talked with a rheumatologist, and it’s recommended I see him. I guess there’s a battery of tests they can do to find out what medication would work best for me. Hopefully, we can figure it out!
Thanks Jen for sharing your experience!! Some other folks have also wondered about seeing a rheumatologist and whether that would help—I hope it does and you can report back what you find out. Can you tell me (by comment on the Doctor Finder page or just by email to me) who is your wonderful ortho? It would be amazing to fill in more points on the map so others can luck into the right doc on the first try!! Thanks!!! Please let us know how the rheumatology visit goes if you follow up with that.
Amy
Hi I was wondering how you are doing?
Hi Jen, thanks for asking; I’m struggling a bit with a relapse, haven’t posted about it yet because I’m still waiting to see how my shoulder recovers.
How are is your shoulder doing and how did your visit with the rheumatologist go? If you have some doctor recommendations, please let me know so I can add ’em to the Doctor Finder page!
Best,
Amy
Any sirva experience after Covid vaccine? Had a slight burning feeling upon injection, no pain on the first day, second day had a lot of pain that subsided a couple of days later. started getting spasms around injection site 10 days after first dose and a month later is from my neck down to my wrist.
Hi, I got my 2nd dose of the Covid vaccine (Madena) on March 17 and then next day I started feeling shoulder pain from my shoulder down to my wrist as well. The pain radiates to both my shoulders.
I just had two injections ( flu and shingles vaccine) in my left arm two days ago. The first injection was the shingles vaccine and I immediately felt a sensation in my entire left arm that can best be described as a short burst of electricity. I mentioned it to the administrator right then and asked if it was possible they hit my nerve. They stated that it was not likely and proceeded with the second injection. There was no sensation with the second injection. I proceeded with my day expecting a mild stiffness in my left shoulder and was shocked to discover about 5 hours later that I was basically unable to move my arm without intense pain that has now lasted for 48 hours. I have now booked an immediate appointment with my doctor to diagnose the problem and hopefully reverse and joint or nerve damage.
It’s too early for me to be officially diagnosed with SIRVA but my ortho doctor said the pneumonia shot I received at a local pharmacy by a pharmacist was likely injected into the bursa. He’s thinking she didn’t hit the nerve, but cannot be 100% sure at this point. Although he says he’s seen several people who’ve had shoulder injuries from vaccines, he didn’t respond as though he knew what SIRVA was when I mentioned it.
The shot was immediately painful and within 7 hours I could not lift my arm and the pain was/is excruciating. I am about to start a dose pack of medrol in hopes we can get ahead of the inflammation process. I have already had two frozen shoulders over 10 years ago, so my doctor feels that will not happen again at least. He said if the nerve was hit, there’s a remote possibility I could have encapsulation occur again. After having experienced that, I pray this does not happen.
It’s beyond ridiculous that the public at large has not be made more aware of this problem or that it’s a possibility. I had never heard of this before, nor that the possibility existed from having an improperly place injection. I asked another pharmacist if she was aware of it and she said it happens more often than we realize. It’s now my opinion that pharmacists are not the correct healthcare providers to give an injection. I’m beyond devastated that I walked into a local Walgreens perfectly healthy and left with a damaged shoulder/arm.
My doctor says I should feel better in a week, if not to make a follow up appointment. I will come back in a month to take the survey on this site.
Looks like I have this, too.
Just under two weeks ago I was in to see my GP for another matter. While I was there, I asked for the flu shot. I have a tattoo on my left shoulder, and I usually ask the person administering a vaccine to miss it. The nurse said, “sure, I’ll just go a little higher”. That has never been a problem in the past. I was seated; she was standing.
The vaccine (not the needle) going into my arm hurt like… something else. I’d never felt anything like it before. The pain began near the site where the needle was depositing the fluid and spread down my upper arm. It continued to hurt for several days, then seemed to be starting to improve. At about day 10 it got bad again. That brings us up to the present.
I have difficulty raising my arm. Crossing my left arm over my body hurts too. The pain is at its worst at night. I feel it from my shoulder down to the bottom of my deltoid. That bit at the bottom of the muscle makes me wonder if there’s nerve involvement.
I enjoy lifting weights, and continued that a bit after the injury. A few days ago, I was unable to do even a warm-up set of bench presses. I’m gathering that “walking it off” might not be a good idea, so I should probably lay off upper body work until I see what’s going on.
Googling “flu shot pain weeks later” brought me to a Washington Post article, which gave me “SIRVA” as a further search term. That got me here and to a bunch of articles in the medical literature.
I’ll go see my doctor this week. It’s a teaching practice, so I expect they will be receptive to diagnosing this properly. (Plus I’m in Canada, so there’s less fear of lawsuits.)
Thanks for the site, Amy!
Hey there, sounds pretty similar to me. I also had pain during the shot that was intense. I remember leaving thinking, “I guess some people are not as good at giving shots as other people,” since it hurt so bad! Like you, for a few days the pain was really bad, then it got a bit better before getting worse again. I’m sorry you’re going through this and I hope your case does not end up being severe. Best of luck and please keep me posted on what you learn from the doctor.
Just noticed that one of the articles listed on the Resources page is from the pharmacy school at the university my doc’s practice is affiliated with. So even more reason to think they’ll take me seriously.
Thanks for the kind wishes, Amy. I’ll keep you posted. And I’ll fill out the survey after I’m a little further along in the process.
Hi. I’m in Canada too (Toronto). Had Covid vaccine 3 weeks ago and, just like you, I saw that she had put the needle in WAY to high (where my shoulder is basically skin and bone). I have been unable to drive properly, sleep properly, appetite loss, unable to do any yoga, can’t undress properly or do hair without a lot of pain, typing hurts; even just keeping my arm in rest position hurts because it’s ‘hanging’ off my painful shoulder. Every move is like a knife on the inside of my shoulder.
How has your pain progressed or receded? Are you feeling any better yet? Did you seek/get medical help? Has resting or exercising it helped? Your insight/feedback would be so appreciated! Thanks in advance. : )
Same for me. The pain was immediate down to my elbow. Coming up on 2 months now. I’ve been through 2 Prednisone packs which help while I’m on it but it comes back 48 hours later. Not sure what the next step will be. At least my doctor is on top of it and it is well documented that it’s all connected to the moment of the vaccine. So frustrating.
Hi! How long were your prednisone doses? I did a burst of 5 days, and then another burst of 5 days a week later.
It helped when on it, but like yours, came back as soon as it was done.
Then I was on a ten day taper and the pain has come back but not as badly as before I went on it the third time. This result lasted a full week before getting back to bad again.
Unfortunately for me it’s my lung doctor prescribing the steroids for my asthma… my ortho doesn’t really understand SIRVA.
Maybe your doctor would consider a longer course… depending on when your injury was it could help decrease the inflammation in a more longterm way?
My parmacy gave me a polio booster injection and within a few days my shoulder has been very painful. Over the last few months I have had physio and several cortisone injections but my shoulder is still painful and basically frozen. I would like for the pharmacy to take some responsibility in all this. What did you do?
Hi Andrew, sorry for the delay in responding. If you’re in the U.S., the pharmacy has no liability and you should consider looking into this:
https://www.hrsa.gov/vaccine-compensation/index.html
If you speak to a vaccine injury lawyer you’ll learn that you do have to have symptoms for 6 months or more to be considered for compensation. The system is pretty screwed up if you ask me, for a lot of reasons (mainly because it does nothing to incentivize the pharmacy where you got the shot to do better, because they’re not liable).
But I would consider going back and talking to them, bringing some papers on SIRVA if you can (there are some good ones about proper injection technique for providers on the resources page, scroll down to the bottom):
http://sirvasurvey.org/resources/
They may not take responsibility but they should KNOW what they’re doing wrong!! Potentially, severe injuries on other people could be avoided in the future if you go back and tell them what has happened to you, and remind them to teach their people to not aim too high!!
There are a few papers on the Resources page that deal with frozen shoulder due to SIRVA, which has a specific diagnosis. I hope you can find a good orthopedic doctor in your area who is familiar with SIRVA (about half of them are and the other half might be dismissive). Check out my advice for a first appointment with your doctor, urgent care, or orthopedist:
http://sirvasurvey.org/talking-to-doctors-about-sirva/
Best of luck,
Amy
I’ve been experiencing this in Canada. The Canadian health care is pathetic and doesn’t care about anyone. I can’t lift my left hand or so anything. I played sports and was so athletic before my flu shot. This is so pathetic that no one takes responsibility for this. I can’t lift my left hand anymore. I’ve lost everything I’ve enjoyed about life. I wish a million times over I didn’t get my vaccine. I hope someone reads this and doesn’t get a “routine” vaccine. Sirva is a million times worse than a flu you may get. I’m so depressed now
Hi Mark. Hi. I’m in Canada too (Toronto). Had Covid vaccine 3 weeks ago and I saw that she had put the needle in WAY to high (where my shoulder is basically skin and bone). I have been in terrible pain. Every move is like a knife on the inside of my shoulder.
How has your pain progressed or receded? Are you feeling any better yet? Did you seek/get medical help? Has resting or exercising it helped? Your insight/feedback would be so appreciated! Thanks in advance. : )
Has anybody had a sensation in their shoulder where you can not relax it and it is in a constant state of tension?
I’m suffering from these symptoms. I’m a 22 year old female. I don’t know who to turn to as this point. I’m in pain all the time.
SIRVA can be extremely, constantly painful. I hope you have the opportunity to find a doctor near you who is knowledgeable, but it can be a real struggle to find someone who knows what SIRVA is. This is the best advice I can give:
http://sirvasurvey.org/talking-to-doctors-about-sirva/
Best,
Amy
My pain is noticeable worse in the evening time, is this common?
I didn’t have that particular pattern; for me I noticed the most pain while trying to type at work, or going for jogs/walking/anything that moved my arm. But it did hurt at night too and affected my sleep as well.
I had an MMR vaccine in May 2019. I didn’t notice at the time any unusual discomfort. I didn’t think anything of it, but around that time I noticed pain in my shoulder. I started physio thinking it was work related (I’m a dental hygienist) sometime in January be and did that until February with no changes. I had IMS and was given exercises. I’ve also done chiropractic care every 3 weeks which I’m still continuing for this as well as maintenance due to my career. I asked my doctor if SIRVA was a possibility and she said no. She did however send me for an ultrasound. I was scheduled to have my ultrasound on April 3rd but they called me today and cancelled due to COVID-19 and have no idea when they will be able to re-schedule. I also had a massage cancelled today as well! I don’t even know if I have SIRVA, but it’s the only thing that makes sense and I feel very alone as no one has ever heard of it…I came across it while googling “can an mmr vaccine hurt months later” ?. I’m so frustrated and don’t know what to try next…especially with everything shutting down due to this virus.
I received my vaccination the end of October 2019. I had the usual “feels like someone punched me in the arm” pain for a week or so. Then the pain never went away. It got progressively worse. Dr wanted to rule out heart—so spent $2000+ on nuclear stress test, cat scan, rays etc. went to a nerve dr and he did an nerve induction. More $$$. I had an MRI which showed bursitis. I googled bursitis and vaccine and that is where i learned about SIRVA. I told my physical therapist who informed my dr. I went to an orthopedist yesterday and got a cortisone shot (hurt so bad) and he confirmed it was bursitis—SIRVA. He said it could take a year or more to heal. I’m so frustrated and in pain. I never had any shoulder problems before all this….
I’m so sorry you’re going through this too, Brenda. Thanks for sharing your experiences.
Amy
My mother just got back from getting her shingles vaccine a few hours ago and her she is experience sharp pain in her upper right shoulder. She has significant reduced mobility in her arm.
She hadn’t been diagnosed yet but we are now waiting for her doctor’s office to call back.
Hi Sophie! It is understandable to be very worried about the possibility of SIRVA with sharp pain and reduced mobility right after a shot, especially if it appears that the shot was too high on the arm. Most of us recognized when we got SIRVA that the shot itself was more painful than usual. I hope very much that your mother is just experiencing a short discomfort associated with the vaccine and that it does not develop into a case of SIRVA. I don’t know about for the shingles vaccine in particular, but I was once advised not to start worrying that unusually intense pain after a shot is SIRVA until a week or two weeks with consistent bad pain. I’m not sure that’s great advice, but it is what I was told, so maybe there is hope that it will be short lived in her case. I think I have heard that the shingles vaccine is extra painful so you will probably get a lot of people telling her to not be worried, but it is only natural to be concerned that something was done wrong when the pain is a lot more than usual for a vaccine. Please keep us updated!
7 years of hell and feeling worse than ever. I hope everyone reading this has better luck than I have.
Both my 18 year old son and I went to our neighborhood pharmacy and each got the flu shot. It has been over a month and we both are in so much pain. It must have been poor placement of the shot. We are feeling all the symptoms you have described.
Today I saw this article and learned the hell I went through three years ago has a name: https://www.nbcwashington.com/investigations/new-push-could-block-covid-19-vaccine-injuries-from-program-that-usually-pays-victims/2415521/
This led me to search for more info on SIRVA, leading me here. Thank you all for sharing your stories and what has helped you. In my case, I became delirious from pain and lack of sleep. All I could do was cry out to God for relief, praying for healing! And that is exactly what I received. Although I still have lingering pain and weakness in that arm, it is bearable and no longer debilitating. My heart goes out to everyone who has had to endure this hell. And it sickens me that so many more will face this in the future. And the HHS seems to want to eliminate the little legal recourse available now, just in time for the COVID vaccinations to begin!
Hi
This is really interesting.
I had a whooping cough jab three months ago to allow me to visit a friend with a young baby.
I bared my arm down to the elbow and looked away. It wasn’t until I looked to see where the Dr was putting the bandaid that I realised the needle had gone in VERY high up on my arm.
Two days later I was in excruciating pain when I reached out to put my bag down on the seat beside me.
It’s been impossible to roll my shoulder back to remove shirts/jackets etc.
I’m now seeing an osteopath and trying to get some relief.
This is a nightmare and Drs should be well aware of what not to do!!
Hi. I am having this problem after my covid vaccine. I had it over 3 weeks ago and the pain is definitely impinging on my life. I’m curious if your pain ever subsided/healed and if you got any medical treatment that helped. If you are better, did resting it or exercising it help? Thanks in advance. : )
Thank you for having this resource… I received the COVID-19 vaccine on new year’s eve and the shoulder pain was unbearable. I can move my shoulder now, thankfully, but certain tasks are still difficult and the pain has spread to my elbow and shoulder/neck.
I knew immediately following injection that she had put the needle in too high, and when I went to take off the band-aid later on, I REALLY noticed how off she was… I have my second dose of the vaccine in a few days and needless to say, I’m scared. I’ve been given the go ahead to get it in the other arm… hopefully I don’t end up with both arms crippled! lol.
Uggh, so sorry you’re in this boat, Jillian! Watch ’em like a hawk on the second go-round and make sure they hit the deltoid properly. I hope your pain in the first shoulder goes away quickly and you don’t have a long protracted SIRVA problem. Please keep us updated.
Amy
Hi. I’m in Canada too (Toronto). Had Covid vaccine 3 weeks ago and, just like you, I saw that she had put the needle in WAY to high (where my shoulder is basically skin and bone). I have been unable to drive properly, sleep properly, appetite loss, unable to do any yoga, can’t undress properly or do hair, etc. Even typing hurts. Even just keeping my arm in rest position hurts because it’s ‘hanging’ off my painful shoulder. Every move is like a knife on the inside of my shoulder.
How has your pain progressed or receded? Are you feeling any better yet? Did you seek/get medical help? Has resting or exercising it helped? Thanks in advance. : )
Sorry I said “I’m in Canada too.” I realize now that you didn’t write that you are. Sorry, I guess I saw it on another comment, but am still very interested in your response! Thanks : )
I’ve filled out the initial survey, because I believe I’m experiencing SIRVA. I’m 3 weeks out from a TDAP and definitely experiencing sudden, sharp, breathtaking pain during sudden actions. The rest of the time is a fairly constant dull ache. I’ve continued moving (fear of frozen shoulder), but will try to limit activities that cause pain. I’ve seen my PCP and she examined the muscle, but definitely wasn’t aware of this. I’ll be introducing it to her.
My question is: is the vaccine still efficacious given in the bursa as it would be if it had been given properly in the deltoid muscle? I have been given the Covid 19 vaccine, but will it work having gone into the bursa?
Does anyone know?
Thanks,
Maggie
That’s a really good question. I wish I knew more. What little I do know is that the effectiveness of vaccines does typically depend on where it is injected. For example, some parts of the body (like the glutes) have more percentage of fat than the deltoid, which makes certain vaccines less effective if given there (i.e., you’d need a bigger volume of the vaccine if you got it in the glutes versus deltoid for it to be equally protective). Vaccines are given in muscles because of the high volume of blood flow and easy transport to the lymphatic system. The structures of the shoulder where people get SIRVA after a too-high shot are not muscles and do not have the same blood flow and properties. I wonder if there is SOME immunological response but just not as vigorous as it’d be in the muscle. One can hope that the second dose will finish what the first one started. If you got SIRVA from a second dose, maybe if you have a pretty unpleasant reaction to the second one like so many people do, it is a good sign that the first dose did its job. But I don’t know. This would be a good question to do more research on.
I have the exact same problem and question. Am scheduled for second Covid injection Feb. 24th. The first injection was administered at a County group for elderly people and doses were given by the hundreds so I do not know who administered my injection. I was told it had to be administered high up on my arm and was ignorant enough to allow it. Immediately after I noticed weakness and loss of range of motion. This lasted for a few days and appeared to recede. However, now two weeks later the pain in my shoulder is extreme and is gradually worsening. Thanks for all the info here. Will definitely get the second injection but with the caveat the injection is placed properly at the site.
Should the second injection be given in the same arm?
Hi Leslie, there’s a very active facebook group for folks with SIRVA–if you are on facebook, look for a group called “SIRVA – Shoulder Injury Related to Vaccine Administration” where this topic is being debated by folks with an active, inflammatory SIRVA response currently going on in one arm. I have seen people argue for both sides–same arm or “good” arm, so I don’t think the debate is settled, unfortunately.
It sounds like most people have chosen the opposite arm, watching like a hawk obviously to make sure it is not injected too high but hits the meat of the muscle. So far I haven’t heard from any of them that they ended up with any problems in the opposite arm. SOME folks have also successfully asked to get the shot in their thigh, but that also depends on the person giving the shot being qualified/able to find the right spot on the thigh as well. Good luck and please join the FB group if you can, and if not, keep us posted here on how it goes for you!!
Amy
I’m in the uk and there is hardly any info about SIRVA here. I had my c19 vac in early jan and have had severe pain in my shoulder and arm since. It has reduced but is still painful
Also I am unable to move my arm properly and have now been diagnosed with rotator cuff injury in that arm!
It’s quite ironic as I’m a nurse in the vaccine centre that gave me my vaccine!
I would like to know the answer to this question as well, I hope someone can answer it.
https://ismp.org/resources/prevent-shoulder-injuries-during-covid-19-vaccinations
it is far better to get the second injection in the thigh opposite side of injected arm. (right arm would be left thigh) if you experience adverse reactions in arm/shoulder.
https://www.cdc.gov/vaccines/pubs/pinkbook/vac-admin.html
Adults (19 Years or Older)
For adults, the deltoid muscle is recommended. IM injections are administered at a 90-degree angle to the skin and, for most adult patients, the skin is spread and the tissues are not bunched. It is acceptable in geriatric patients to grasp the tissue and “bunch up” the muscle. As with children and adolescents, the vastus lateralis muscle in the anterolateral thigh is an alternative site if the deltoid sites cannot be used.
Thanks for these resources, Jennifer. Where did you see that it is better to do the second injection in the thigh opposite of the injected arm? I’d like to find that reference. I just finished writing up a post before seeing this comment, that describes some of this, but I had not heard or seen the “opposite” part before! Thanks!!
Have you been feeling any better yet? I had my covid vax 3 wks ago and am in agony. Now I guess I’ll have to go to the Dr. Here’s an article with a Dr. saying that if the vax goes into the shoulder joint/bursa, that you do not get covid antibodies and need to do BOTH injections over again! That’s when I started crying. I’m in Canada. : (
Whoops, here’s that article: https://www.detroitnews.com/story/life/advice/2021/03/16/dr-roach-covid-vaccination-causes-long-lasting-pain/115562656/
I believe I have SIRVA following the 2nd dose of COVID vaccine on 2/14. During both shots I experienced dull but severe pain immediately as the needle was inserted, and it worsened as the vaccine was injected. Both shots were delivered in the same arm and both were very painful — like a very hot needle was inserted into the capsule and delivered very hot liquid. In the evening after the 2nd injection, my arm was nearly incapacitated with pain during night and for the next few days. On about the 4th or 5th day, the pain subsided to what now feels like a torn rotator cuff (can an injection tear a RC?) and now on the 9th day the pain is the same. The injection site is very high on my arm, barely a finger width below the top of my shoulder. Some activities are very painful and others are less so if done with care. I’m planning to take a wait-and-see approach for a few weeks. About 12 years ago I had a minor RC tear in the same shoulder, so I am familiar with that type of pain and wondering if the shots aggravated that or caused a new injury.
Male, 70 years young. I am also diabetic type 1 and on 4 insulin shots a day – not afraid of needles. Two years ago I had a flu shot in my left deltoid and suffered with pain and not being able to lift my arm. My wife had to help me get any pullover shirts on or off. It resolved pretty much after a year, but made me very anxious about IM vaccine administration. Next flu season I asked my doctor if they could administer it in my dorsogluteal site ( not the words I used) and all went well without pain. Today I am scheduled to get my Covid vaccine and my best guess is to go for the right arm. Any advice appreciated – wish me luck.
Hi Bob, I have heard of people asking and receiving the covid vaccine in the dorsogluteal site (good word!), but it probably depends on the person administering the shot. I don’t believe there is research yet about whether the vaccine is calibrated to give you full efficacy when given there, but I don’t know why it would be different than getting another vaccine in the leg.
Other folks have also asked the question of whether they should get the covid vaccine in which arm. I will say that so far it sounds like folks who have/had bad SIRVA cases have gotten their covid shots, and a properly administered covid shot seems to be fine for folks who’ve had SIRVA before. So the choice of arm depends to some extent on whether you’re willing to risk your dominant arm—but in theory it should not be a risk at all, just make sure they identify the deltoid properly! I am way down on the queue for getting my covid shot but when it’s my turn I plan to ask for it in the hip and if they won’t give it to me there, get it in the left arm but watch ’em like a hawk.
I’m in the uk and there is hardly any info about SIRVA here. I had my c19 vac in early jan and have had severe pain in my shoulder and arm since. It has reduced but is still painful
Also I am unable to move my arm properly and have now been diagnosed with rotator cuff injury in that arm!
It’s quite ironic as I’m a nurse in the vaccine centre that gave me my vaccine!
I received my second Covid vaccine dose on February 18th and felt immediate pain that only worsened over the next 48 hours with limited range of motion. Two days after that dose, I noticed a lump in the middle of my arm, about 3-4 inches under the injection site(which was given very high on my shoulder). I saw a GP 3 days after the vaccine and she told me it was probably SIRVA, but the lump could be a torn bicep tendon. She sent me for an X-ray which showed shoulder impingement and “spontaneous bicep rupture”. I have never had any pain/issues with my shoulder and am in generally good health at 48. I’m scheduled with ortho on March 1st, but I’m afraid they will try to say it’s not related to the vaccine. I honestly don’t know how it couldn’t be with the exact symptoms and pain I’ve experienced so far.
Oh, my goodness, I’m so sorry. You have a right to be worried that they may not believe it is vaccine-related; a lack of knowledge and skepticism about SIRVA is extremely common.
I’d strongly recommend you bring a few papers about SIRVA into your appointment with your orthopedist on March 1 and be prepared to discuss them if your doctor is unaware and skeptical. It sometimes works. My advice about that is here:
http://sirvasurvey.org/talking-to-doctors-about-sirva/
I’m going to dig deeper and look for papers in the research that mention biceps damage specifically. With SIRVA, many different things can be damaged depending on what the shot hits and how the body responds.
I searched through the published literature for mention of biceps RUPTURE and didn’t find any, though I have no doubt that yours is a very bad case of biceps tendon damage leading to rupture. Here is an article about a very bad case of SIRVA where the biceps tendon was damaged (see p.e285, “In addition, the extensive humeral head chondrolysis and biceps tendonitis were likely an inflammatory reaction to the injection”:
https://pdfs.semanticscholar.org/1421/177b3442d039a5cd82b9eeb1185ecf15145a.pdf
Here’s another one you should bring that mentions the biceps:
https://www.racgp.org.au/afp/2016/may/don%E2%80%99t-aim-too-high-avoiding-shoulder-injury-related-to-vaccine-administration/
And this one:
https://pdfs.semanticscholar.org/c239/e0a861cd16268fcbb79a1b5ec1b9496006ff.pdf
Thank you so much for this information, Amy! I did see reference in the second article of a 73 year old female patient who presented with rotator cuff tear and bicep tendon rupture. I’m glad I will be informed and somewhat prepared for appointment on Monday.
Ah, great, glad you read it more carefully!!! I just skimmed this time and missed it. Best of luck. I really hope the ortho is a good one. If they are, please let me know so I can add them to the Doctor Finder page.
I’ve had terrible SIRVA symptoms after my 2nd Covid vaccine on February 2nd. I work at a hospital and it was administered by an ER doctor during an employee vaccine clinic. I was wearing a bulky coat and slipped it off right before sitting down in front of the doctor. As a thin 52 year old woman, I have rather “boney” shoulders. Perhaps the doctor thought I was heavier and used a longer needle than needed? In any event, there was intense pain at injection and I noticed the site was higher than usual for injections. I feel at fault myself for only nudging my shirt off my shoulder due to modesty issues as there were about 15 other people in the room with no privacy curtains. I’m on my second day of prednisone with much relief but fear the pain will return once the coarse is over.
Sorry you have gone through this. I had my covid shot 3 wks ago and I am in so much pain it’s impeding on my life. I guess I have to go to the Dr., but I half expect no on to believe me. Has your pain/problem improved at all? Feedback would be great. Thanks in advance.
Oh and forgot to say… I have very ‘boney’ shoulders too and she injected me super high on the shoulder where, when you touch there, all you can feel is skin and bone underneath. I’m not skinny elsewhere on my body, so maybe she thought I was chubby and assumed my shoulders have muscle but it’s actually bone. I’m so scared to be unable to do things properly without pain and be unable to workout/yoga.
Frozen shoulder sufferer here from the Influenza vaccination I received on September 18, 2020. The pain has been excruciating!!! I have had two cortisone injections that have relieved the pain but only last about a month or two. About to call the Orthopedic for a third one because the pain has become unbearable again. This has been the pits for sure!!! At night is the absolute worst since I can’t get comfortable and therefore I only manage a couple of hours sleep a night. I was super hesitant to get the Covid vaccine but jumped in anyway and had them inject in my “sirva” arm(was not willing to risk use of both arms)!!!!
Uggh, yes, it is the pits!! Sorry you are suffering so much. So glad you got the Covid vaccine anyway. From conversations with lots of SIRVA sufferers who have gotten theirs so far, no one has reported a second or worsening case of SIRVA from getting it done (of course that doesn’t count people who got their SIRVA from the Covid shot to begin with). Please keep us posted on your recovery.
Hello all. I had a tetanus shot in my right arm in Januaty of 2021 and ever since my right arm has been so very painful. I cannot reach behind me or across to even touch my left shoulder. I cannot lift heavy items or push myself up off the couch. It feels like the initial ache and pain/burn of the shot but its not going away. Its really affecting my life. I cannot sleep comfortably on either arm. If i sit up or lay flat i have some relief but thats not realistic. This is so miserable.
Hello
I’ve just found this website after not knowing what do do for almost 4 weeks of searching and trying to find out if a vaccine can cause injury which I’ve never heard of before but having read and read the symptoms makes sense . When I had my 1st covid-19 vaccine it was really quick and I was anxious so probably didn’t relax my arm and it took seconds but pinched when the needle came out and it hurt
I didn’t think anything of it
Until the next morning a Sunday I felt like I had layed on my arm all night
I still over 3 weeks later can’t lift anything can’t lift my arm up
Everyday tasks are painful and the tingling, numbness and weakness and pain is very frustrating if it’s not better the nurse said I’ll need physical therapy
I’m hoping it’s not an injury but it’s definitely worrying .
REPLY
Had the 2nd Moderna vaccination in left shoulder Feb 22, 2021 and have had excruciating pain since then on both sides of upper left arm, shoulder, and trapezius, plus spasms, and tingling that radiates throughout the entire impacted area; the hard knots described by others is especially painful. Took Prednisone (orally) for 10 days and pain was gone for awhile, but returned. My Dr. diagnosed it as a “pinched nerve” in my neck. Have experienced pain from pinched nerve sporadically for many years, but it only lasts a few days and is no where near the pain I’ve been in for the past 2+ months. Have taken Motrin and Percocet to reduce pain, but it’s a temporary solution.
I’m so surprised to discover there’s a name for this—SIRVA—and grateful for the affirmation from others who’ve experienced or are experiencing it. And, it’s encouraging to know that there are treatment options.
I received a flu shot in 2013 and could not use my left arm for about a year. I had no insurance and did not go to a doctor. I recently had both Covid shots. I had no problems, but I woke up one morning and could not use my right arm! It felt JUST like how my arm felt after the flu shot. BUT, I did not get the Covid shot in my right arm! I figured if I had a problem I’d rather it be with my left arm so I got the shots in my left arm. Is it possible that the vaccines themselves can cause SIRVA? Has anyone else experienced this? I thought I was crazy when I had SIRVA with the flu shot, but this exact pain in a non-shot arm?
I received my second dose of the Moderna Covid-19 vaccine on 04/23/2021. When the nurse put the needle in my arm, I immediately told her “my God it feels as if you just gave me a cortisone shot”. It felt like it went right into my shoulder joint. I went home and have been suffering with excruciating pian ever since. I have no insurance. I finally went to a doctor after 3 long weeks. They diagnosed me as having possible SIRVA. I was given a shot of cortisone and given a steroid pack to complete at home. This helped some but, now that this treatment is complete now just 2 days later the pain is back and worse. I am getting a referral to an Orthopedic Dr. And will keep everyone posted. The pain I am feeling is in the shoulder joint and radiates down the right side of my arm causing burning, weakness, tingling and numbness all the way to my fingertips. Just getting started with this nightmare I am facing. God bless this site. I will keep all who suffers this tragedy in my prayers. I will update as my treatment progresses.
Hi Carmen. I just had my COVID vaccine 3 wks ago and have been in serious pain since. She put the shot in way too high on my boney shoulder. Logic would say it went right into my joint. I’m curious if time has improved your case, or not. Did you get any medical treatment other than the cortisone? Did anything help? In your opinion, does forcing yourself to move the shoulder (eg. work out) improve it, or does resting it (even such as a sling) help? Which one is better? Thanks in advance. : )
Hi, had the Johanssen vac on April 24 – no pain – but hellish pain started 10 days later. Is this possible? I woke up with it, might have slept awkwardly or lifted something too heavy the day before, but still on and off very painful – the symptoms seem identical to SIRVA, but is the gap too long before the pain starting to be it?.
Regards
Thank you all for sharing your stories. I live in Ontario. I had my second covid vaccine beginning of June. Within days I was in the ER due to the excruciating pain and not being able to move my arm. Doctor who saw me never heard of SIRVA. He gave me sling and said I would be referred to an orthopaedic surgeon. Saw orthopaedic surgeon a week later. He never heard of SIRVA either. Prescribed Celebrex and physiotherapy. Will see him in 5 weeks again. No one has done an ultrasound or X-ray yet. I have requested my family doctor send me for an ultrasound. Just waiting for the appointment. My physiotherapist is the one who suggested it. Will wait and see. Still painful. I have been off work for two weeks now. I do not think anyone believes this is real. Thanks for listening and sharing. ?
Hi Tracie. I’m in ON as well (Toronto). Had the covid vax 3 wks ago and have been in terrible pain since. I’m scared the Dr.s won’t believe me or want to admit so. Has your case improved since you wrote this? Did you have medical treatment? In your opinion, does trying to move it more (eg. working out) or resting the arm (eg. sling) help? I’m so scared about how bad this is and could get. Thanks in advance. : )
Hello Kate. Sorry for the late reply. I thought I was getting better, but I am getting sharp shooting pain now. I haven’t mentioned this to my doctor yet as I think he will think I have lost my marbles. I know initially he had to report it to Public Health. I have appointment with my doctor in a couple of weeks and I am going to mention the pain. I got my third shot in my other arm without any issues. My pharmacist did it. They were the ones who knew what SIRVA was initially. How are you feeling?
Thanks for this website, I have experienced 2 months of on and off pain on my right shoulder after receiving 2nd Covid shot. I went to consult a doctor then was told could be caused by vaccination shot, then I discovered the name for it. The doctor didn’t suggest much treatment nor even MRI scan than just rest well. Hopefully my condition will get better soon.
Hi Daniel. Has your shoulder improved? I had my vaccine 3 weeks ago and have been in terrible pain since. Did anything help you? Does moving it help more, or resting it (such as wearing a sling and trying to immobilizing it)? Did you have medical treatment? Thanks in advance. : )
I got my first Covid vaccine four weeks ago. I was very nervous getting the vaccine and felt it was administered quite low in arm. By the next day my shoulder blade felt like it was karate chopped. I went to the doctor who said it could be frozen shoulder and gave anti – inflammatory and advised Physiotherapy. No relief from dry needling or medication, the pain worsened and started radiating down to my elbow and wrist. When sitting or driving it feels like I have a blockage trying to push through my veins. Does anyone else have this? Went for my second vaccine, explained pain for previous 4 weeks and it was given in a much higher position on shoulder bone. I feel so helpless that the pain will not go away!
Hi everyone. I live in the UK and have been experiencing severe pain in my arm since my COVID vaccine in April this year. The pain is progressively getting worse and I can no longer swim or climb. I experience sharp severe pain with certain movements such as reaching, although my arm has recently begun to ache at rest. It is also affecting my sleep. I saw a physiotherapist who advised me to exercise my arm but to stop if too painful, which it is. I have another appointment next week. He suspects the needle was injected into bone and the site where the shoulder muscles attach to the bone. The vaccine was administered quite low in my arm and felt very deep. It’s so debilitating that it’s starting to really get me down. It’s great to have found this site and hear about the different experiences. I will follow avidly and post any useful updates in relation to any treatment / diagnosis I may receive.
I got SIRVA with a flu shot September 2020, effects almost immediate after a couple of hours & severe for several days/weeks. I saw an orthopedist a month later when the somewhat diminished pain was still a big issue for me. When gathering materials for a lawyer 5 months later, I noticed he didn’t mention the vaccination at all in his medical report, just that I had a rotator cuff injury, nothing was observed by xray.
After several months (5) I discovered SIRVA & contacted a lawyer. Although the severe pain had diminished, I still experienced sharp pains & lack of flexibility when my shoulder tries certain movements.
I saw another orthopedist a few months later since the first offered to do a CAT scan only if I was to have surgery on my shoulder. It is now 13 months after the vaccination & I wonder if having an MRI would show anything or if it is too late now, too long after the injury? I don’t know if a negative result after 13 months would hurt my case since there would no concrete evidence connecting the flu shot to my pain & limited movement, just a report of a rotator cuff injury 1 month after a flu shot.
Hey Jeff, I don’t know all the answers to your questions, but I do know that my lawyer told me that the vaccine court doesn’t penalize petitioners for their doctors having no clue about SIRVA. I was worried about that too. That is, (????), hopefully the fact that the first doctor or even any later ones don’t mention the connection, or even if they don’t agree with it, the fact that the problem (rotator cuff injury) began after vaccination is enough (and even if there was no MRI at the time). I think the court must be aware of the lack of awareness and skepticism among providers.
Best of luck, Amy
James in Saskatoon Saskatchewan Canada … not pro needles or pain meds for anything but bowed to 1st Covid vax to keep my business alive. Next day shoulder pain 3-4-5 and no strength and cannot raise elbow chest high. Toughest part is am side sleeper and wake up every few hours. NO advice from Sask Health other than get 2nd shot in other arm which freaks me out. Almost 90 days later. Found this link from a Medical Nurse in Portland USA. Have been to chiropractor and massage weekly with very little if any —- relief. October 2021
I have SIRVA and I have been doing therapy for over six weeks now. Still struggling
Has anyone tried acupuncture to relieve the symptoms?
I’m pretty sure what I’m experiencing is SIRVA. Shoulder pain started 2 days after injection and now 10 days in its getting worse every day. Burning, aching and I cant raise my arm above shoulder height. Forget about putting on a seatbelt.
A guy named Dr. Bodor at Napa Medical Research has a technique called debridement (www.sciencedirect.com/topics/medicine-and-dentistry/debridement) which sound promising but is still experimental I believe. You can contact the guy at http://www.bodorclinic.com
We are delighted to say that we have been serving the local plumbing needs in Bristol for many years, working to solve plumbing problems for residents and small businesses alike.
The technician turned up exactly on time and put in a full days work.
Newly formed government and industry collaboration set strategy
for recruiting an additional 100,000 construction workers a
year.